On the Cutting-Edge
Cancer cell immunity in the crosshairs: worth the expense?
It’s time to say goodbye to ineffective and costly cancer treatments. Japanese scientists have found unique genetic alterations that could indicate whether expensive immune checkpoint inhibitors would be effective for a particular patient.
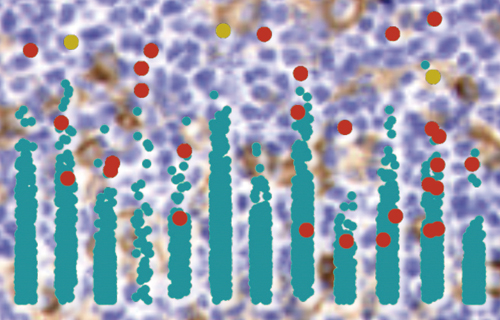
Programmed-death ligand 1 (PD-L1) is a protein that tells the immune system not to kill a particular cell. Publishing in Nature, a recent study reports that genetic alterations affecting a part of the PD-L1 gene increases the production of the protein, allowing cancer cells to escape detection by the immune system.
“This is the first study to illustrate that a structural abnormality in the 3' untranslated region of the PD-L1 gene causes an abnormally high production of PD-L1 protein, consequently aiding cancer immune escape,” says one of the lead authors, Keisuke Kataoka, at Kyoto University. “Our study suggests that whether or not a cancer has this particular abnormality could be a good indicator of its response to immune checkpoint inhibitor drugs.”
Antibodies that target PD-L1 or its receptor PD-1 have shown remarkable therapeutic effects for many cancer patients, sometimes even for those who are terminally ill. Treatment using such antibodies is extremely expensive, however, and oncologists are keen to find a biomarker that can predict the effectiveness of these drugs for individual patients.
“We identified PD-L1 structural alterations affecting the 3' untranslated region of the PD-L1 gene in 27% of patients with adult T-cell leukemia/lymphoma by analyzing next-generation sequencing data,” explains senior author Seishi Ogawa.
Prompted by this initial finding, the team searched for similar structural alterations in sequencing data from a total of 10,210 samples deposited in the Cancer Genome Atlas.
“Through this analysis, we found that such abnormalities were found in many common cancer types, including malignant lymphoma, as well as stomach and cervical cancers. We also generated human and mouse cells having a similar structural alteration using the CRISPR-Cas9 genome editing system, and confirmed that these cells actually showed an elevated expression of PD-L1 protein and were able to escape the immune attack,” says Ogawa.
“To test the importance of such structural alteration as a genetic marker, a phase two clinical trial is ongoing at Kagoshima University and other institutions,” adds Ogawa. “Once we confirm the significance of these genetic alterations, it’ll be a game-changer for immunotherapy in cancer.”